Deep learning for obstructive sleep apnea diagnosis based on single channel oximetry
Overview
Obstructive sleep apnea (OSA) affects more than 20% of the global adult population, with approximately 80% of cases remaining undiagnosed. Although home sleep test solutions have existed for almost two decades, they suffer from significant limitations. A recent review reported a misdiagnosis rate of 39% for home sleep tests. Previous academic attempts to develop OSA detection approaches using oximetry have been inconclusive due to either moderate performance or limited validation (often limited to a single cohort).
What was the approach to solving the problem?
We hypothesized the possibility of accurately diagnosing OSA using nocturnal continuous oximetry only. To test this, we conducted an extensive retrospective, multi-center analysis of a total of 12,923 polysomnography (PSG) recordings, representing 115,866 hours of continuous data from six independent databases. Our deep learning model, named OxiNet, was trained on one dataset and evaluated on the remaining five, effectively accounting for crucial distribution shifts across variables such as age, sex, ethnicity, and co-morbidities. We benchmarked OxiNet against a machine learning model using the oxygen desaturation index as input and a second machine learning model using digital oximetry biomarkers (see here as input.)
What NSRR data were used?
We used the SHHS, CFS, MROS, and MESA datasets available on the National Sleep Research Resource (NSRR). We also used a private dataset, denoted UHV, obtained from the sleep clinic at the university of Valladolid.
What were the results?
OxiNet demonstrated remarkable performance, missing only 0.2% of all moderate-to-severe OSA cases, while the best benchmark algorithm missed 21%. Although no major error was made on the external test set, the performance of OxiNet was impacted by a distribution shift in ethnicity for the Black and African American participant subgroup as well as individuals with concomitant chronic obstructive pulmonary disease.
What were the conclusions and implications of the work?
The study conclusively proved the feasibility of single-channel oximetry analysis powered by AI for diagnosing OSA. It represents a significant milestone, culminating two decades of intensive research efforts aimed at answering the question of whether a robust OSA diagnosis could be achieved using a single oximetry sensor.
How does the tool work?
The OxiNet algorithm takes as input the nocturnal oximetry time series. The digital oximetry biomarkers (OBM) can be computed on variable window sizes relative to the intended use.
How can researchers use/benefit from the tool?
The OBM open-source library is available with a thorough documentation and user interface here. A version of OxiNet is available here.
Resources/multimedia
Publication on OxiNet
Related publication on oximetry biomarkers
PhysioZoo open-source resource
Youtube tutorial to the PhysioZoo SPO2 user interface usage
Paper Summary
To drive health innovation that meets the needs of all and democratize healthcare, there is a need to assess the generalization of deep learning algorithms for underrepresented groups and across various distribution shifts thus ensuring that these are robust for all. This retrospective study is, to the best of our knowledge, the first to develop and assess the generalization of machine learning and deep learning models for obstructive sleep apnea (OSA) diagnosis from the sole continuous nocturnal oximetry channel.
To conduct this research, we used a total of 12,923 polysomnography (PSG) recordings, representing 115,866 hours of continuous data from six independent databases, five of which are available at NSRR. The models were trained on the Sleep Heart Health Study (SHHS) first visit and evaluated on five external test sets that factorized important distribution shifts across age, sex, ethnicity and co-morbidity.
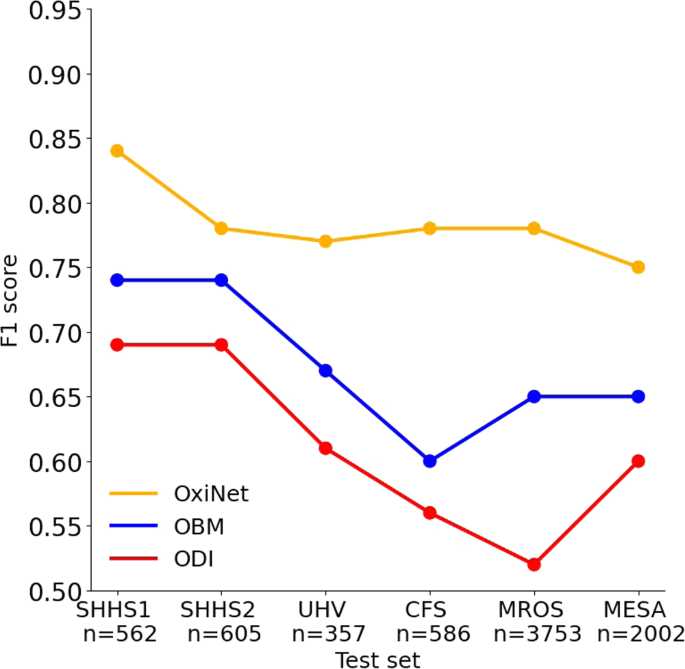
Our findings demonstrate that our new deep learning algorithm, denoted OxiNet, significantly outperformed benchmark algorithms on all external test datasets in a significant and non-incremental manner. Specifically, 0.2% of all moderate to severe patients were missed using OxiNet while 21% of moderate-to-severe patients were missed using the best benchmarked algorithm. OxiNet performance dropped on the external test sets but this resulted in no major misclassification. The main drops in performance on the external test sets were due to distribution shift in ethnicity for Black and African American and comorbidity for individuals with concomitant chronic obstructive pulmonary disease. This is coherent with recent reports on the effect of dark skin pigmentation on the accuracy of oximeters readings.
This large retrospective, multi-center analysis provides strong support for the clinical usability of single-channel oximetry analysis for OSA diagnosis powered by AI. It also provides a unique example of how large open source-databases can enable the assessment of generalization of novel machine learning and deep learning algorithms across ethnicity, age, sex and co-morbidity thereby ensuring the creation of robust and fair data-driven models.
F1 score for each model as a function of the test set.Authors
Blogpost Author: Dr. Joachim Behar
Paper Authors: Dr. Jeremy Levy, Dr. Daniel Álvarez, Dr. Félix Del Campo, Dr. Joachim Behar
Citation: Levy, Jeremy, Daniel Álvarez, Félix Del Campo, and Joachim A. Behar. "Deep learning for obstructive sleep apnea diagnosis based on single channel oximetry." Nature Communications 14, no. 1 (2023): 4881. https://www.nature.com/articles/s41467-023-40604-3